Concerns 'very small number' of Scottish mesh survivors will be granted permission for US removal surgery
A contract has been signed allowing women from Scotland to travel to Dr Dionysios Veronikis’ clinic in Missouri for transvaginal mesh removal surgery.
The news comes after hundreds of women were left with painful, life-changing side effects when they received the implant surgery.
Advertisement
Hide AdAdvertisement
Hide AdThe contract will cover surgery for mesh removal and associated costs such as travel and accommodation – all paid for by the NHS.

However, Dr Wael Agur, who represents the views of mesh-injured women at the Scottish Government’s mesh complications working group, has concerns “gatekeeping” will take place over the America trip.
The independent advisor said the decision to go to America for mesh survivors is not solely theirs to make as NHS Scotland’s Greater Glasgow and Clyde specialist team has to agree to the decision.
The Complex Pelvic Mesh Removal Service was established in NHS Greater Glasgow and Clyde and the service assess needs and “where appropriate”, performs mesh removal surgery.
Consultant gynaecologist and honorary professor with the University of Glasgow, Dr Agur said: “There have been calls for the Scottish Government to ensure adequate surgical skills in mesh removal in Scotland since January 2019.


“Essentially, the Glasgow team is the gatekeeper and may not want a large number of these women to go to the US so I expect the Government will support the Glasgow Health Board on this.
“I expect a very small number of women will be allowed to go.”
The Scottish Government said they have decided “exceptionally” to offer those affected by mesh complications “a wider range of service choices than would be normal” in the provision of NHS health services.


Advertisement
Hide AdAdvertisement
Hide AdA Scottish Government spokesperson said: “When there is agreement between the patient and her clinicians that removal surgery is the appropriate course of action, the decision on where to have surgery is entirely for the patient to take."
However, Dr Agur, said the use of the word “exceptionally” worried him, adding: “No obstacle should be put in a woman’s way to go out of the country.”
Publication of an out-of-country clinical referral criteria has been recommended by Dr Agur so that woman have a clear understanding of their surgical pathway.
Mesh implants were suspended in Scotland in 2014 "in all but exceptional circumstances", before being halted completely in 2018.
One woman told The Scotland on Sunday she was “very frustrated” and “shocked” when she heard mesh implants were being offered to her and others when she moved to Scotland.
After suffering from debilitating pain from mesh she had implanted in 2007, the survivor, who moved to Scotland in 2013, had specialist removal surgery in 2012 in America.
Margaret* is still impacted by the mesh through scarred tissue and greater susceptibility to infection, however, her debilitating pain was relieved post-removal operation.
Margaret, who lives in the Edinburgh area, said: “When I came here, I went to a medical specialist and they suggested doing a (second) implant and I was like, ‘You’ve got to be kidding me?’”
Advertisement
Hide AdAdvertisement
Hide AdThere are two main reasons why surgical skills in Scotland have “lagged behind” America when it comes to mesh removal, according Dr Agur.
One, the initial denial that the mesh is causing such severe problems. And two, the continuation of mesh implantation, despite the Government suspension, which led to loss of trust and, therefore, the lack of patients to operate on to build experience.
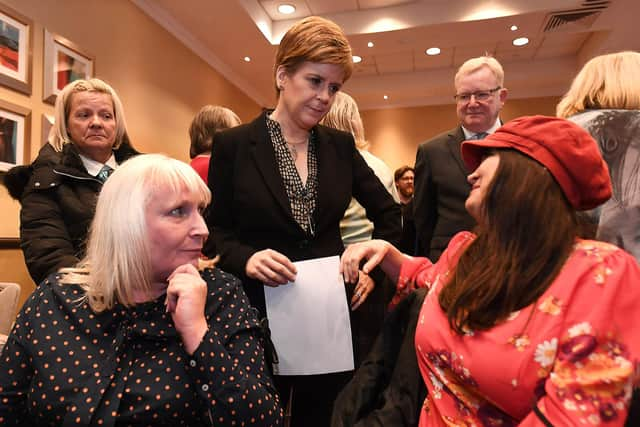
In Scotland, Dr Agur said women reported being told by surgeons the mesh tape was completely removed but they found out later that the tape was only partially removed. Nicola Sturgeon has commissioned an independent review into medical records on this which is currently ongoing.
“Continuing to implant mesh devices despite the government suspension did not help the trust in mesh removal in Scotland amongst the injured women. It’s a no-brainer for many women to go somewhere else.” said Dr Agur.
Dr Agur believes training from Dr Veronikis in Scotland would have “accelerated” the surgical skills in Scotland. However, he said the Glasgow team did not engage with the offer of supervised training as it would be “an admission that their skills need to be brushed”.
Health Secretary Humza Yousaf said the overall cost of the mesh scheme was expected to reach £2m to £3m. This includes reimbursements for women who have already paid for private surgery.
Dr Agur said: “Training here would have accelerated the learning curve of our surgeons and they would have achieved excellent surgical skills in a much shorter time and regained the women’s trust.
“In my view, had the offer by Veronikis to come here been accepted by the Glasgow team, all this taxpayer’s money funding women’s treatment in the US would have been saved.”
Advertisement
Hide AdAdvertisement
Hide AdScottish Conservative MSP Jackson Carlaw, who campaigned on behalf of women affected by mesh, welcomed the US trip announcement from the Government, however, he shared Dr Agur’s concern over gate-keeping.
The MSP said: "What we want to do now is get women there as quickly as possible due to the pro-longed suffering. Dr Veronikis is the surgeon women have confidence in.
"There has been a professional snobbery within the NHS about the sub-contracting of any healthcare to Dr Veronikis but the blunt truth is the surgical experience simply hasn’t been proven to exist in Scotland.
"I and other MSPs will be champions of anyone who feels they are being denied access as we go forward.”
Margaret said: "This is a big, loud screaming example of lack of care shown to women’s health in particular. There isn’t any government doing enough for women’s health.”
A Scottish Government spokesperson said: “Anyone seeking mesh removal is encouraged to first discuss this with their local clinicians within their own Health Board. If considered appropriate at that stage they will then be referred to the NHS’s Complex Pelvic Mesh Removal Service in Glasgow, for consideration by a full multi-disciplinary team. If it is agreed that surgery is appropriate, the patient can choose to be treated by the service already available in NHS Scotland or to be referred to a specialist NHS centre in England or to one of the independent providers. Any patient can, of course, also seek a second opinion, and their GP will be able to advise on this.
“Case review by the multi-disciplinary team is pivotal in ensuring that all clinical considerations are taken into account in the planning of surgery that meets the needs of the patient concerned. This process has been agreed to by the private providers, and is intended to ensure that the patient is fit for surgery, that all relevant diagnostic investigations have been undertaken and, importantly, that there is proper integration with all pre- and post-operative care provided locally, by the NHS in Scotland.”
*The name of the mesh survivor has been changed for safe-guarding reasons.
Comments
Want to join the conversation? Please or to comment on this article.
