Irene Oldfather: Giving patients a say in their treatment

It is encouraging to see the policy narrative around the future direction and ambition of the NHS fully embracing the concept of people as partners in their own health and wellbeing. Recent documents such as the National Clinical Strategy and Realistic Medicine firmly place shared decision-making between patients and clinicians and principles of self-management very firmly at the heart and core of future engagement.
Since 2013 the Alliance’s People Powered Health and Wellbeing programme has been working with disabled people, people who live with long-term conditions and unpaid carers to influence and contribute to the delivery and improvement of support and services – including peer support, which people report being hugely beneficial.
Advertisement
Hide AdAdvertisement
Hide AdThe importance of this is now widely recognised across health and social care and will be a key driver of the National Clinical Strategy. Understanding what matters to you instead of what’s the matter with you, is entirely different. The focus on improvement in the NHS has led to the development of the “Five Must-Dos” which describe what good clinical engagement should look like.
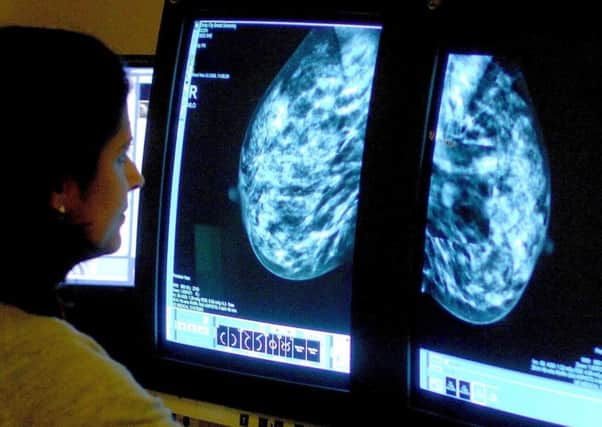
A King’s Fund article on patient preferences noted that doctors believe that 71 per cent of patients with breast cancer, rate keeping their breast as a top priority. But the actual figure reported by patients is 7 per cent (Lee et al, 2010). Furthermore, doctors believe that 96 per cent of breast cancer patients considering chemotherapy, rate, living as long as possible a top priority. But the actual figure reported by patients is 59 per cent. Asking people what matters and who matters has to become a routine part of the business of clinical interaction, as does establishing what outcome the patient wants.
This personal outcomes ethos also runs through the innovative Our Voice programme of which the ALLIANCE and Scottish Health Council are key partners as it seeks to enable and facilitate purposeful engagement as a step towards transforming health and social care. Utilising feedback and opinions from across Scotland the Our Voice framework can create a mutually beneficial partnership between people who access support and services and those who deliver them.
New thinking across the NHS is predicated on working towards an approach which supports people accessing healthcare to be fully informed and encouraged to understand options about their own care and treatment. This may include identifying interventions which are of limited value or indeed may in themselves cause harm.
The new approach will also require moving from a strictly medical model of care to acknowledge the importance of wider social interactions, reducing isolation, encouraging physical activity and joining peer support networks.
In Scotland, the House of Care model represents a tangible and proven approach that allows health and social care to embrace care and support planning, and fulfil its responsibilities to support self-management with people living with long-term conditions.
Creating conversations about health and wellbeing need not always fall to the GP. The role of the wider practice multi-disciplinary team can be constructive and free up GPs for more complex care and treatment. The Alliance’s National Link Worker Programme operating in some of the most deprived areas of Glasgow has demonstrated that having space to talk through problems is a huge part of the solution.
According to George Bernard Shaw, the single biggest problem with communication is the illusion that it has taken place. There is a challenge to arrive at the place where constructive and equal conversations and shared decision-making take place, but reaching the destination could be literally life changing.
• Irene Oldfather is Director at the Health and Social Care Alliance Scotland and a UK Member of the European Economic and Social Committee.