The changing face of HIV and AIDs in Scotland, as told by TV advertisements
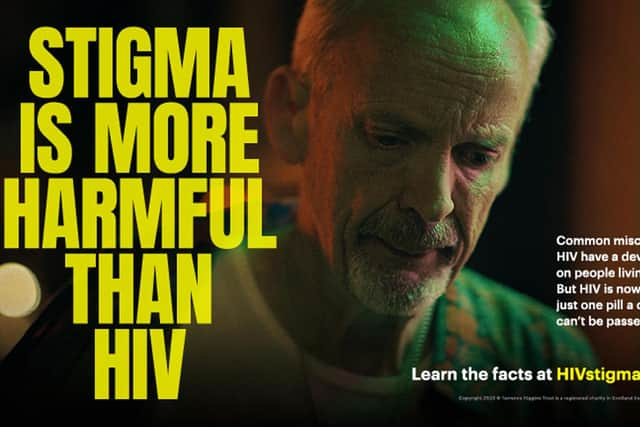
The first major TV advert on HIV in Scotland, since the UK Government’s infamous ‘Don’t Die Of Ignorance’ campaign, is now airing – but HIV infection in Scotland looks very different than it did in the 1980s.
The notorious advert aired 40 years ago and featured falling tombstones, as well as warning viewers that HIV was a “deadly disease” with no known cure.
Advertisement
Hide AdAdvertisement
Hide AdInstead, the new advert, which launched on STV on Monday night, informed viewers those with the disease can live a healthy and happy life. The changing tone of the adverts reflects the drastic changes in HIV infection and treatment over the past 40 years.

Similar to today, police in 1980s Scotland could not stop the drug trade. Back then, however, police aggressively targeted drug paraphernalia – needles.
Unlike in Glasgow, which introduced needle exchanges, this led to the widespread sharing of needles in Edinburgh. There were reports of singular needles being shared between entire streets.
This led to an explosion in HIV, at a time where retroviral drugs were not yet sophisticated enough to prevent AIDs. Young, otherwise healthy heroin users in the city became ill, and soon began dying. The deaths were treated as purely drug deaths.
A blood test for HIV, previously thought to be a disease that only affected gay people, soon shone a light on the cause of the deaths. It was a GP from Edinburgh’s Muirhouse area, Dr Roy Robertson, who made the connection by testing blood samples given by drug addicts during a hepatitis C outbreak.

More than 50 per cent of Edinburgh’s addicts turned out to be infected with the virus, making it the capital of Europe’s AIDs crisis. In comparison with the rest of the UK, few cases of HIV in Edinburgh were attributed to homosexual transmission.
According to research from the University of Edinburgh, between June 1987 and June 1988, reported cases of HIV infection in Edinburgh increased from 1,239 to 1,504. Of these figures, about half were due to intravenous drug use; a quarter to homosexual sex; and the final quarter to contaminated blood products and other routes of transmission.
The spread of HIV among Edinburgh’s drug-using population, and among gay men in the rest of Scotland, helped spread prejudice against sufferers of the disease.
Advertisement
Hide AdAdvertisement
Hide AdIn the early stages of Scotland’s HIV epidemic, little was known about the routes of transmission. And even when the pathology of infection became known to the medical community, misinformation persisted in the general population.
In April 1987, Princess Diana shocked the British public by shaking the hand of a man suffering from AIDs, without gloves, publicly challenging the notion that HIV was passed from person to person by touch. We now know that HIV attacks the immune system, causing a chronic, life-long infection that can be managed successfully by antiretroviral therapy.
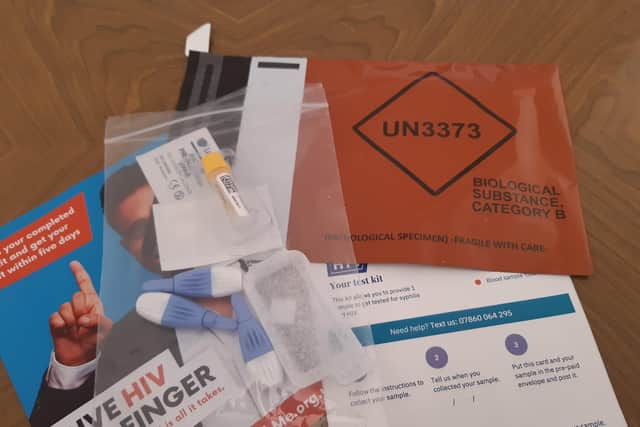
According to Public Health Scotland (PHS), HIV can be transmitted through condom-less vaginal and anal sex, sharing injecting equipment and transmission from mother to baby during pregnancy, birth or breastfeeding.
While untreated HIV infection progresses to advanced HIV disease or acquired immune deficiency syndrome (AIDS), modern day treatments mean the life expectancy of someone contracting the disease today is comparable to people without HIV.
However, ignorant attitudes to the disease persist. Scottish Government-funded research, carried out by YouGov, found “worryingly low levels of knowledge about HIV”.
Just one third (35 per cent) of people in Scotland would be happy to kiss someone living with HIV, despite it being known since the 1980s that HIV can’t be passed on through saliva. The data also shows almost half (46 per cent) of people in Scotland would be ashamed to tell other people they were HIV positive.
The data shows a clear lack of knowledge regarding the progress made in the treatment of HIV. People on effective treatment for HIV cannot pass the virus on through sexual contact, and would even produce negative HIV blood tests.
Despite this, just a third of Scots are aware that people living with HIV and on effective treatment can’t pass it on to partners.
Advertisement
Hide AdAdvertisement
Hide AdThe prejudice and fear of the 1980s doesn’t tally up with the reality of present-day HIV infection in Scotland.
According to PHS, in December last year there was an estimated 6,600 people living with HIV in Scotland, of whom 6,150 (93 per cent) had been diagnosed.
Research from PHS found for the first time in over a decade, new HIV diagnoses among heterosexuals were higher than for gay and bisexual men.
Last year in Scotland, 42 per cent of all new HIV diagnoses were in heterosexuals, compared to 29 per cent in gay, bisexual and other men who have sex with men (GBMSM)
According to the Terrence Higgins Trust (THT), “whilst GBMSM remain more impacted by HIV relative to population size, targeted interventions in this group have led to one of the big success stories of the epidemic”.
The introduction of PrEP – pre-exposure prophylaxis – can reduce the risk of getting HIV from sex by about 99 per cent when taken as prescribed.
A spokesperson for the THT said: “The steep decline of 37 per cent since 2017 in new HIV diagnoses among GBMSM is partially attributed to uptake of the HIV prevention pill PrEP among this group, who between July and December 2022 accounted for 85 per cent of first-time prescriptions.
“It’s also thanks to accessible HIV testing, condoms, health promotion and people living with HIV’s adherence to treatment, which suppresses the virus and means it can’t be passed on to partners.”
Advertisement
Hide AdAdvertisement
Hide AdAs well as PrEP, post-exposure prophylaxis (PEP) is “highly effective” when taken within 72 hours of an exposure to HIV, and is also partly responsible for the reduction of HIV infections among the GBMSM demographic.
On December 1, 2020 – a date that marked World Aids Day – the Scottish Government set the goal of ending HIV transmission in Scotland by 2030.
Comments
Want to join the conversation? Please or to comment on this article.