Mutant protein key to athlete heart deaths puzzle

Hypertrophic obstructive cardiomyopathy (HCM) is an inherited disease where the muscle wall of the heart becomes thickened.
Sportsmen and women who have the condition can put themselves at risk by building up the muscle wall so much the heart cannot take the strain thus stopping the normal flow of blood going in and out of the heart resulting in sudden cardiac arrest.
Advertisement
Hide AdAdvertisement
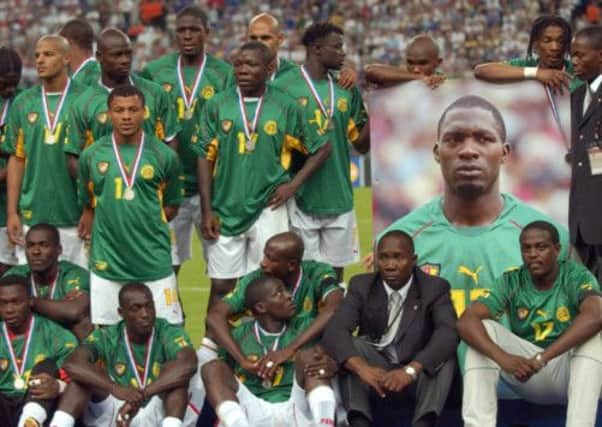
Hide AdFabrice Muamba, the Bolton Wanderers central midfielder, was treated by a heart specialist who was among the fans after he collapsed on the football pitch last March, as a result of the condition. However, Cameroon footballer Marc-Vivien Foe died on the pitch in 2003 after suffering a sudden cardiac arrest due to HCM.
But now a Harvard Medical School study suggests the condition - referred to by some medical professionals as “hocum” - can be prevented from developing for several months by reducing the production of a mutant protein.
Those with HCM have been born with one of the walls of the heart thicker than it should be. It is estimated that 1 in 500 of the UK population has the condition.
While there is no cure at present treatments can be given to help control symptoms and prevent complications.
Christine Seidman, professor of medicine and genetics at Harvard Medical School, whose study is published in the journal Science, said: “There’s really no treatment for HCM right now. You can treat symptoms like chest pain or an arrhythmia, but that’s not getting at the fundamental problem.
“While the application of this strategy is in the very early stages, it shows considerable promise.”
The study found of more than 1,000 different mutations that can cause HCM have been identified across about 10 genes that make heart muscle proteins.
People with HCM have one “good” copy and one “bad” copy of one of those genes.
Advertisement
Hide AdAdvertisement
Hide AdStudying one of the mutations that causes particularly severe disease researchers targeted the analogous “bad” gene in mice while leaving the “good” gene alone.
The researchers created an RNA interference (RNAi) tool designed to home in on the single HCM-causing mutation and stop it from making its harmful protein.
They packaged the RNAi inside a virus - a common RNAi delivery technique - and injected it into lab mice engineered to develop HCM.
They compared the results to two untreated groups of mice, one with the same HCM mutation and one without.
By suppressing the “bad” gene, the RNAi was able to reduce production of the mutant protein by about 28 per cent.
That was enough to prevent development of HCM manifestations - including ventricular wall overgrowth, cell disorganization and fibrosis or scarring - for about six months, or one-quarter of the mice’s lifespans.
Prof Seidman said: “For all intents and purposes, the heart looked normal. Wonderfully, boringly normal.”
The treatment successfully targeted heart cells in the mice without affecting other organs.
Advertisement
Hide AdAdvertisement
Hide AdAlthough it did not reverse any existing HCM damage, halting the progress of HCM would be a significant advance in itself.
Prof Seidman added: “If somebody already had a certain amount of wall thickness and you prevent it from worsening, that would be a step forward to limit progressive symptoms and development of heart failure.”
The research could also help advance treatments related to another genetic condition called dilated cardiomyopathy, where the heart becomes baggy and thin-walled and contracts too little instead of too much.
The researchers now plan to investigate whether they can continue to delay HCM in mice with booster shots, reverse disease damage or reduce HCM-related arrhythmias.
Sarah Dennis, information manager for the Cardiomyopathy Association, gave the research a cautious welcome.
“There are some promising elements in this research. But it is still in its very early stages and a long. long way from helping people.”