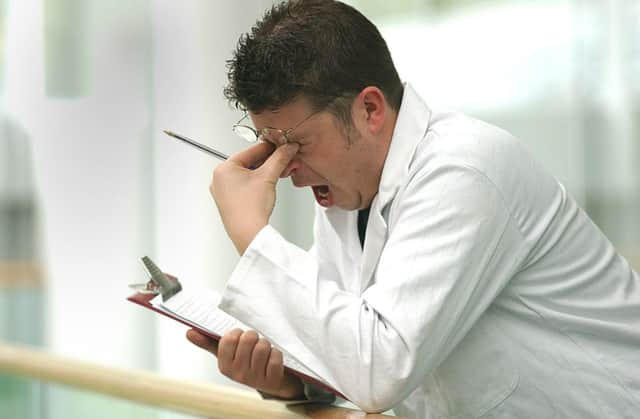
Doctors buckling under workload warns leader

The “inexorable rise” of management has also come under fire from Dr Brian Keighley, chairman of the British Medical Association in Scotland, who said doctors had to be listened to more.
He said the NHS was struggling to deal with the pressures of an ageing population, Westminster-led funding cuts and rising expectations from patients which include a shift towards a seven-day-working week in hospitals. Dr Keighley said that despite the Scottish Government protecting the NHS in Scotland from the austerity cuts seen south of the Border doctors still faced growing financial constraints.
Advertisement
Hide AdAdvertisement
Hide AdHe warned that the fall in hospital bed numbers over a period of years was leading to a rise in waiting lists and more pressure on Scotland’s Accident and Emergency departments.
And the crucial contact between doctors and patients has particularly suffered, Dr Keighley warned in his New Year message. He said: “Reports of stress and burnout amongst all grades of clinical staff are now emerging across the service.
“An ageing population, increasingly sophisticated technology and pharmacology, legitimate rising expectations from patients and their families, the expectation of consistent levels of patient care over all seven days of the week and faster access to treatment are all pressures with which the Scottish Government and its 14 health boards have struggled over the past year.”
The “inexorable rise of managerialism” in the NHS has been a “major cause of dysfunction”, he added, and there is a need to return to clinical priorities.
In his message, he said: “I disagree with suggestions that managerial and process change holds the solution to sustaining high quality care and believe instead that it is only by working with doctors and other healthcare professionals that a solution will be found.
“The steady reduction of hospital beds contrary to medical advice and without a wider whole-system approach, has led to the inevitable but predictable assertion that it is an intrinsic lack of capacity which has resulted in rising waiting lists and pressure on accident and emergency over recent years.”
New contracts are now being proposed for doctors, along with “radical” changes to training and greater weekend working and Dr Keighley insisted doctors are ready to look at new ways of working to improve patient care.
But he said any overhaul of the current system should only take place when there is a “clear indication that these changes will produce sustainable benefit and not merely shuffle the deckchairs”. He added: “There is already a danger that the existing workforce is limited in its ability to generate and deliver solutions because of exhaustion with current arrangements.”
Advertisement
Hide AdAdvertisement
Hide AdA recent BMA survey of doctors found eight out of ten believed the pressure of their work load was “high” or “very high”.
The doctor’s concerns follow a report by nursing leaders which found many nurses are forced to work unpaid overtime to meet patient needs.
A majority of nurses say they think patient care is suffering because of the pressure they are under.
Labour in Scotland has called for a review of NHS provision after it emerged that several hospitals operate a skeleton staff cover at weekends, although the Scottish Government has set out plans for more of a seven-day operation.
Labour’s health spokesman, Neil Findlay, said: “The picture painted by the BMA will be reflected in patient experiences and it is not a good one.”
The NHS in Scotland has been protected from the worst of the austerity cuts and still enjoys a record budget of £11.8 billion. Between 2010-11 and 2015-16 the resource budget will have risen by 2.1 per cent in real terms.
Last night, a Scottish Government spokesman said waiting times and waiting lists are close to a ten-year low and figures showed 95 per cent of A&E patients are seen within the target of four hours.
He said: “Patients and clinicians are at the heart of achieving excellence in healthcare and that is why, unlike the UK government, we are investing in the NHS and protecting budgets.
Advertisement
Hide AdAdvertisement
Hide Ad“We also are investing £50 million through our unscheduled care action plan to improve the way emergency care is delivered across NHS Scotland.
“Having the right number of staff in the right place at the right time is about more than staff numbers.
“We are committed to improving efficiency and freeing up time for clinical care. Management plays an important role in achieving this.”
Case study: ‘General practice is unsustainable as a full-time job’
Over the last five years I’ve noticed a constant and incessant rise in the demands placed on GPs but we are expected simply to get on with it. No resources are put in place to help manage this extra work.
I found this incredibly stressful. I would arrive at work at 8am every day and often not leave before 7:30pm or later. I dreaded going into work. I felt like I was constantly treading water and keeping my head afloat. The more stressed I got the more detached I became from my patients. I would get more and more frustrated with patients who brought in lists of problems. I would be ratty with them. I stopped sleeping well. I often woke in the night and remembered things that I had forgotten to do. I also felt incredibly guilty. I wasn’t the doctor I wanted or aspired to be. I wasn’t the compassionate, empathetic person that I used to be. I joined a fitness class but rarely made it on time during the week and was left with only being able to attend at weekends, which decreased my ability to de-stress further.
After talking at length with colleagues and my husband, I was lucky that they agreed to support me and I decided to drop to three days a week. I feel great.
I’m taking my time with patients. I don’t mind if I run late now, I don’t mind if they need to talk. I think general practice, as it stands, has become totally unsustainable as a full-time job.
• Dr Amy Smart is a GP principal, in East Lothian
SEE ALSO