How big data is being used to improve our health
This article contains affiliate links. We may earn a small commission on items purchased through this article, but that does not affect our editorial judgement.


Their pioneering work and legacies live on in improved nursing, standards of cleanliness in our hospitals, and computational and analytical techniques in data and population health. The passion, commitment and breakthroughs these two women made in the fields of computing and analytics more than 150 years ago are part of the process that led towards “big data” today.
Nightingale was a champion of using healthcare statistics to highlight problems and potential solutions, but she was also the recognised pioneer in creating tools for visualising this information in order to help others understand it. She created a variant of the pie chart - known as a polar area diagram - to eloquently identify and strikingly illustrate to civil servants the problems in medical treatment of soldiers during the Crimean War.
Advertisement
Hide AdAdvertisement
Hide AdThe process of collating large amounts of statistical information - or data - and packaging it into a chart - or visualisation - which may reveal wider patterns or insights which could in turn save lives, reduce waiting times, or simply save money has been around in healthcare since Nightingale’s innovations. Combined with today’s computing and networking power, “big data” is promising a revolution in our nation’s health, care and wellbeing service.


On an individual level, utilising big data in healthcare can pave the way towards personalised, pre-emptive advice and warnings that can ultimately lead to better health and improved quality of life. But before we get to the outcomes, how do we go about harnessing the power of this data?
One of the biggest perceived obstacles facing healthcare organisations looking to move with the technological times in terms of how they handle data, is patient trust. Taking advantage of public or private cloud services might make sense from an operational point of view, but for the individuals served by these organisations, how and where their data is stored is an important factor. Recent high-profile data breaches, lack of awareness and education around the differences between the various methods of data storage and access, does not help with this issue of trust and organisations must work hard to assure individuals that their data is safe.
Yet this is a somewhat curious situation. Every time an individual does internet research, shops online or uses a loyalty card somewhere for example, they are creating personal information about them that they neither own nor control. This data is captured, combined with that of countless others (big data) and then processed to deliver personalised recommendations, special offers, or other relevant services based upon their habitual behaviour and activities. People are content with this level of data usage if it can deliver them added value. So what could be more valuable to a person than their own health and wellbeing?

In today’s connected world, health professionals, care workers, families and citizens are all increasingly able to collect significant amounts of data, including medical data; using Fitbit, Microsoft Band, smart watches, monitors and a range of other health devices. In each case, there are major opportunities for innovation, for collaborative working and for businesses and citizens to contribute to improvements in services.
Underpinning all of this needs to be a secure, scalable and reliable platform, allowing for all this information to be managed on a level where trust can be established and maintained between those creating the data and those responsible for safeguarding and making sense of it. The cloud is where this can happen.
Progress in turning big data into service delivery improvements will need the trust of citizens, and co-creation between the different participants. Citizens expect data to be protected by the medical providers, and place high trust in GPs. Maximising opportunities for innovation will come when citizens, businesses and service providers find areas of collaboration.
Advertisement
Hide AdAdvertisement
Hide AdData can be aggregated, matched to other data sets and generate insights into citizen science, health and wellbeing information. Imagine if the power of the crowd that is gathering this data could also store it, and give consent for it to be used to treat citizens. With its remote geography, and constantly improving connectivity Scotland is well placed to implement new health services and to work with big data analytics to shift resources to prevention and improve the health, care and wellbeing of citizens.


Data being analysed by the NHS National Services Scotland is related to the logistics and planning of healthcare; Matt Lovell, CTO at Pulsant in Edinburgh predicts big changes in the way data directly pertaining to patients’ health is collected and processed.
“Wearable technology is hugely beneficial in terms of capturing routine data - blood pressure, for example - to systematically record the patient’s recovery process, and that technology will advance quite quickly now in terms of the amount of data that it can collect - with the patient’s permission, of course.”
This could lead to quicker diagnoses, he says, but could also save the health service money – especially when it comes to Scotland’s remote communities. “In outlying rural communities where it’s much harder and much costlier to bring patients to doctors, we could see the increased use of wearable technology to capture information, to proactively monitor that information and obviously have an alert system that triggers a preventative or a proactive response from medical professionals. I think that is one of the greatest benefits that we will see emerging over the next 12 to 24 months from wearable technology.”
Imagine combining this sort of early warning system with a digital heath service that allows patients to quickly have an online, recorded consultation with a doctor using Skype for Business - who is already able to see all sorts of pertinent information about the individual and make more informed and appropriate initial treatment decisions. Waiting rooms would no longer be filled with patients, travel costs would be reduced, more patients could be seen per day, and more people who would otherwise struggle to get to a doctor in good time could then be diagnosed sooner.
In Wales the DAWN project in the rural north has been using Skype to empower diabetic patients in Gwynedd for some years. This has transformed and simplified services, and patients find the process less stressful and more convenient.
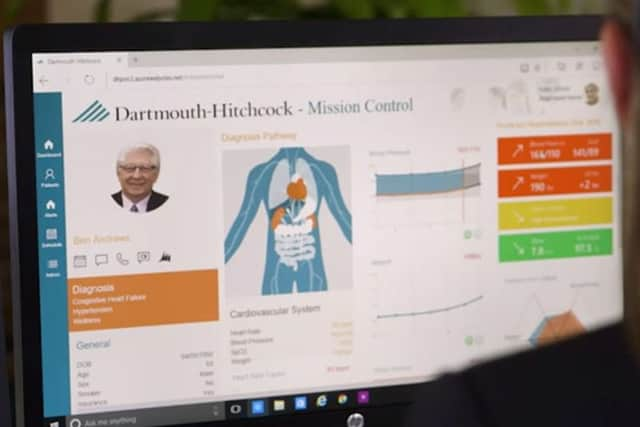
In other parts of the world, data is being used to support hospital systems, design, operations and citizens. There are significant investments in new systems and innovations. Ethan Berke, Medical Director at Dartmouth Hitchcock Hospital in north east USA talks about their innovation – Imagine Care. The Hospital has invested in a range of new services and technology to empower patients, and to allow physicians, family and care workers to support the treatment and care of citizens.
This focus on personalised care in the USA has a range of equivalent policy innovations in Scotland – person centric health, care and wellbeing, self-directed support and self-management. Innovation and knowledge transfer from other systems will be essential if Scotland is to tackle the challenges in working with big data to improve health and care outcomes.
Advertisement
Hide AdAdvertisement
Hide AdHealth research in Scotland has a long history, and big data is a major area of focus. According to Dr Mike Capaldi, Director of Commercialisation at Edinburgh BioQuarter, the bioscience community set up by Scottish Enterprise, the University of Edinburgh and NHS Lothian: “Big data analytics is the process of extracting useful information from huge amounts of data.”
“Traditional stability testing in the laboratory can be very time consuming, typically eight to 12 weeks. Comparable tests on a supercomputer take about 45 minutes. So addressing the challenge of big data is not a ‘nice to have’ – it is a fundamental enabling competence.”
Fortunately for Scotland, it is home to a healthcare data resource and network that is envied around the world, having started to adopt electronic health records nationwide some years ago. According to the Scottish Government’s 2011 e-Health Strategy paper: “Existing systems for linking individual patients’ hospital records have supported a wide range of groundbreaking population health and clinical research, and this has generated intense interest, in Scotland and elsewhere, in extending linkage to other health records, such as primary care and prescribing data, and to non-health records, such as education, income, census and survey data.”
Today’s statistical experts supporting NHS Scotland have advanced technology to call upon. National Services Scotland (NSS) operates at the heart of NHS Scotland, collecting millions of records on hospital admissions, GP visits and prescriptions every year. It recently brought in a new software system to help NHS Scotland’s various departments analyse, present and dissect the health body’s extraordinary wealth and depth of data.
According to Phillip Couser, Director of Public Health and Intelligence at NHS National Services Scotland, there is a real push within the NHS to make more use of data in order to drive efficiency.
“The NHS is under pressure from a variety of factors; an aging population, advances in clinical care which is increasingly expensive and public spending constraints.
“Against this background it is crucial to use NHS data to ensure that services are delivered in an efficient and safe way.
Matt Lovell sees a culture of healthcare data excellence thriving in Scotland, thanks to collaboration and funding, not to mention The Data Lab, a recently established collaboration in Scotland between industry, government and academia set up to help drive, develop and support innovation driven by data science.
Advertisement
Hide AdAdvertisement
Hide Ad“I think Scottish organisations outside and including The Data Lab have benefitted from the development of the Edinburgh BioQuarter and medical research funding,” he says. “Institutes such as the Farr Institute have benefited from and are nurturing the pools of technical competence and capability in and around big data and associated tools and techniques needed to analyse the data and apply understanding and knowledge to the data.”
Those three areas - improved healthcare, improved responses and reduced costs - are imperative to the health service, especially in this era of austerity. A move to cloud services not only provides the wherewithal for organisations to reduce costly overheads associated with the current methods of data storage and management, but also opens that information up to wider application within the context of big data. Both of these can deliver tangible improvements within healthcare, from facilitating speedier, remote diagnoses, right through to larger portions of budgets being able to reach the frontlines where patients can feel a significant impact.
“The challenge now is to harness the potential of technology and big data to move from a retrospective view of health service activity to a predictive view of health outcomes.”
While few could argue with the benefits of such developments, patient confidentiality and security is a worry for many people - especially with high-profile data breaches becoming a fairly regular item in the news. Scotland is moving more and more data to Cloud services and this enables the innovation at scale, security and service improvements required to support business and public services regardless of geographic location – as well as providing the computing horsepower required to collate and analyse the huge amounts of data now generated in our day-to-day lives.
Big data is only a part of the innovation – health and care is a complex system, and many other layers of data from health, care and well-being will be generated and potentially shared with local authority, third sector service providers, private sector care homes, nursing staff and other participants. Person centred policies and delivery also mean that citizen centric, trusted data sharing models are likely to evolve to enable individuals to participate as well.
The NSS’s Phillip Couser insists that the groundwork carried out by both the healthcare service and the Farr Institute should keep patient data secure in the four regional Safe Havens and one National Safe Haven that have been established. Referring to the online servers, or “clouds”, where such data is stored, he says: “The NHS in Scotland and the Farr Institute have invested heavily in recent years to ensure that we have powerful and secure IT platforms that allow for the processing of big data. This ensures that patient privacy is maintained whilst also getting the very best from our national data resources. We believe that this is what the public expect of us.”
While Nightingale and Lovelace could never have predicted that the use of data and computers in healthcare would enable such innovation in the age of the supercomputer and cloud computing, they would surely still look on with some pride that the basic principles and innovations of computers, data analysis and visualisation pioneered more than a century ago are still helping patients today. That sense of pride would be matched with similar feelings of excitement about what will be possible in the near future, based on what has been accomplished in such a relatively short period of time through the adoption of a more technology-lead approach to healthcare through the use of big data.
Case Studies
Data and Innovation in the American Health System
In New Hampshire, USA the Dartmouth-Hitchcock Health System is piloting a highly coordinated, intensely personalized solution built on Microsoft technologies for harnessing big data using machine intelligence and advanced data analytics, including Microsoft’s Cortana Analytics Suite.
Advertisement
Hide AdAdvertisement
Hide AdThe innovation and investment is seeking to deliver safe, high quality personalized care. Some of the innovations include analytics suite – interfacing with providers and patients, use of machine intelligence and learning to monitor health status; data gathering, modeling, prediction and monitoring.
Big data techniques are also being used in gathering dynamic updates, and advising the staff on potential care pathways and decision making advice.
Scotland Research, Health and Big Data
Researchers are using computer-generated modeling, simulations and big data analytics to create better products, get greater insights and gain competitive advantage over traditional development processes by getting to market sooner – with more innovative designs.
The Scottish wing of the Farr Institute, based at Dundee Medical School and in Edinburgh’s BioQuarter, is a collaboration between six Scottish Universities and NHS National Services Scotland with the goal of simultaneously improving health standards while making Scotland a world leader in health data research. Its aim is to set “the international standard for the safe and secure use of electronic patient records and other population-based datasets for research purposes”.
According to Mike Capaldi of BioQuarter, the institute’s research will lead “to advances in preventative medicine, improvements in NHS care and better development of commercial drugs and diagnostics. It will also provide new insights into the causes of certain diseases for which there are currently no cures.” While the very name “BioQuarter”, might seem far removed from patient care and the average hospital bed or GP waiting room, Matt Lovell of Pulsant believes that innovation in the sector is intimately linked with the healthcare we all receive from the NHS.
“You are getting the benefit translated back to improved healthcare, improved responses from healthcare and reduced costs. These are the three key areas that in the last 12 months and the next 12 months a lot of NHS Scotland organisations and supporting organisations are really looking to address with the help of big data and the investment in big data and cloud computing.
“I’m not saying ‘solve’ because I think it’s an ongoing exercise. I think this is a case of creating focal points of where data can immediately benefit NHS Scotland and patients in those three areas.”
NHS National Services Scotland and Big Data
Michael Muirhead, head of business development at NSS, says: “A lot of the data that flows through the NHS comes to our organisation. And we’re responsible for the definition, the collection, the collation, and dissemination of all this information to support the NHS as it carries out its duties.
Advertisement
Hide AdAdvertisement
Hide Ad“Our department provides a range of functions, for example, blood transfusion, the payment to doctors, GPs, dentists and pharmacists, national IT infrastructure and procurement, a whole range of things. We’re in a sense the national information collection agency for the NHS in Scotland.”
The software’s modern interface and visualisation tools allow Muirhead’s colleagues in the NHS to study, “slice and dice” and really get under the skin of data that might otherwise be too dense for all but a devoted statistician to digest.
“Our mission statement is turning information into evidence for action to support the health and well-being of the people of Scotland,” says Muirhead. “And in that journey from data to information to translational intelligence is really important for us and we see Tableau as being really a crucial component of the armoury that we have to allow us to achieve that.”
Matt Lovell adds: “All cloud systems that are supporting NHS Scotland are what’s called ‘private clouds’. This means that they are dedicated in all aspects of their function to supplying only services to NHS Scotland and NHS healthcare organisations and that’s the same for Pulsant and any other service provider in Scotland.”
And he believes that while being able to share patient records between different NHS departments with watertight security - and the patients’ consent - represents a huge challenge, it will surely be worth the effort.
“Being able to secure records between different departments and services will lead to a better patient experience but we have to be clear and transparent in how those are communicated. But it is a very complex picture when you’ve got many departments, different geographies having to share data and you need to get the approval of patients to share it.
“Being clear on why the information is being shared and which departments it is being shared between is important to maintaining patient trust and I know that there are some very dedicated and committed individuals who are working extremely hard to communicate that message to the wider communities,” he adds.
According to Phillip Couser, Director of Public Health and Intelligence at NHS National Services Scotland, there is a real push within the NHS to make more use of data in order to drive efficiency.
Advertisement
Hide AdAdvertisement
Hide Ad“The NHS is under pressure from a variety of factors; an aging population, advances in clinical care which is increasingly expensive and public spending constraints.
“Against this background it is crucial to use NHS data to ensure that services are delivered in efficient and safe way.
“Scotland has some of the best data in the world and National Services Scotland uses this to help NHS Boards and the Scottish Government to monitor and plan services. The challenge now is to harness the potential of technology and big data to move from a retrospective view of health service activity to a predictive view of health outcomes.”
- This article was produced in partnership with Microsoft